- The DeFlame Diet
- Supplements
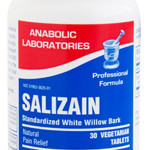
- Salizain (white willow bark extract)
- Salizain and Basic Health Program
- Salizain and Advanced Health Program
Far too many people suffer with chronic pain. Multiple factors participate in pain expression, so if one is looking for a magic bullet (drug or supplement), in most cases, he/she will be out of luck. Pain is complex and must be attacked on multiple fronts. Primarily a DeFlaming diet is very important to avoid “feeding” the pain. The pro-inflammatory foods listed in the DeFlame Diet Book function to “feed the pain.” For more details about how diet “feeds” the pain, The DeFlame Diet book contains a clear explanation.
From a supplementation perspective, the Basic Health Program supplements are typically adequate for supporting the DeFlaming dietary recommendations to achieve a “deflamed” state that often renders people free of pain or less compromised by pain.
The addition of probiotics, Coq10, and botanticals/spices in the Advanced Health Program supplement suggestions are often very beneficial to more thoroughly deflame the system.
Regarding a specific supplement, white willow bark has been shown to reduce pain expression. In the case of low back pain, it is comparable COX-2 inhibitors (Vioxx) and regular NSAIDs. And white willow bark has a better safety profile with side-effects being similar to those of a placebo. Go to the Salizain page to learn more about white willow bark.